Some lung cancers may be discovered through screening, however most lung cancers are diagnosed because they are causing issues. The real diagnosis of lung cancer is done by looking at a sample of lung cells in the lab. If you have suspected signs or symptoms of lung cancer, visit your doctor.
Your doctor will inquire about your medical history to learn about your symptoms and any risk factors. Your doctor will also check you to search for symptoms of lung cancer or other health concerns.
If the findings of your history and physical exam indicate you could have lung cancer, additional testing will be done. These might involve imaging studies and/or biopsies of the lung.
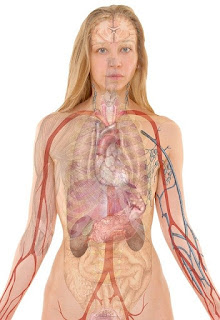
Imaging tests employ x-rays, magnetic fields, sound waves, or radioactive chemicals to make photographs of the interior of your body. Imaging studies could be done for a variety of reasons both before and after a diagnosis of lung cancer, including:
Chest x-ray.
Chest x-ray employs a very tiny dosage of ionizing radiation to obtain photographs of the interior of the chest. It is used to examine the lungs, heart and chest wall and may be used to assist identify shortness of breath, persistent cough, fever, chest discomfort or damage.
Computed tomography (CT) scan.
A computed tomography (CT) scan combines a series of X-ray pictures collected from various angles around your body and utilizes computer processing to generate cross-sectional images (slices) of the bones, blood vessels and soft tissues within your body. CT scan pictures give more-detailed information than standard X-rays provide.
A CT scan has various purposes, but it's especially well-suited to swiftly assess patients who may have internal injuries from automobile accidents or other sorts of trauma. A CT scan may be used to view almost all regions of the body and is used to detect illness or damage as well as to plan medical, surgical or radiation therapy.
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI) is a form of scan that employs high magnetic fields and radio waves to obtain detailed pictures of the interior of the body. An MRI scanner is a huge tube that incorporates strong magnets. You lay inside the tube throughout the scan.
positron emission tomography (PET)
A positron emission tomography (PET) scan is an imaging examination that may assist show the metabolic or biochemical activity of your tissues and organs. The PET scan employs a radioactive substance (tracer) to reveal both normal and abnormal metabolic activity.
Bone scan.
A bone scan is a nuclear imaging technique that helps identify and monitor numerous forms of bone disease. Your doctor may recommend a bone scan if you have unexplained skeletal pain, a bone infection or a bone damage that can't be detected on a conventional X-ray.
Tests to identify lung cancer
Symptoms and the results of some tests may strongly imply that a person has lung cancer, but the official diagnosis is done by looking at lung cells in the lab.
The cells may be obtained from lung secretions (mucus you cough up from the lungs), fluid extracted from the region surrounding the lung (thoracentesis), or from a questionable spot using a needle or surgery (biopsy) (biopsy). The decision of which test(s) to apply depends on the context.
Sputum cytology
A sample of sputum (mucus you cough up from the lungs) is examined at in the lab to discover whether it includes cancer cells. The easiest method to accomplish this is to acquire early morning samples 3 days in a row. This test is more likely to help discover malignancies that originate in the main airways of the lung, such as squamous cell lung cancers. It may not be as useful for discovering other forms of lung cancer. If your doctor suspects lung cancer, more testing will be done even if no cancer cells are identified in the sputum.
Thoracentesis
Whether fluid has formed around the lungs (called a pleural effusion), physicians may remove part of the fluid to find out if it is caused by cancer spreading to the lining of the lungs (pleura) (pleura). The accumulation could also be caused by other illnesses, such as heart failure or an infection.
For a thoracentesis, the skin is numbed and a hollow needle is placed between the ribs to drain the fluid. The fluid is tested in the lab for cancer cells. Other tests of the fluid are also occasionally beneficial in identifying a malignant (cancerous) pleural effusion from one that is not.
If a malignant pleural effusion has been detected and is causing problems breathing, a thoracentesis may be repeated to remove additional fluid which may assist a person breathe easier.
Needle biopsy
Doctors commonly use a hollow needle to acquire a tiny sample from a questionable region (mass) (mass). An benefit of needle biopsies is that they don’t need a surgical incision. The problem is that they take just a tiny quantity of tissue and in certain situations, the amount of tissue removed could not be enough to both establish a diagnosis and to run further tests on the cancer cells that can help physicians chose anticancer medications.
Fine needle aspiration (FNA) biopsy
The doctor uses a syringe with a very thin, hollow needle to remove (aspirate) cells and tiny bits of tissue. A FNA biopsy may be done to examine for malignancy in the lymph nodes between the lungs.
Transtracheal FNA or transbronchial FNA is done by inserting the needle through the wall of the trachea (windpipe) or bronchi (the big airways leading into the lungs) during bronchoscopy or endobronchial ultrasonography (explained below) (described below).
In certain cases a FNA biopsy is done during an endoscopic esophageal ultrasonography (described below) by inserting the needle through the wall of the esophagus.
Core biopsy
A bigger needle is used to extract one or more tiny cores of tissue. Samples from core biopsies are generally selected since they are bigger than FNA biopsies.
Transthoracic needle biopsy
If the suspected tumor is at the outer part of the lungs, the biopsy needle may be placed through the skin on the chest wall. The place where the needle is to be put may be numbed with local anesthetic beforehand. The doctor then guides the needle into the spot while looking at the lungs with either fluoroscopy (which is like an x-ray) or a CT scan.
A potential risk of this technique is that air may leak out of the lung at the biopsy site and into the gap between the lung and the chest wall. This is termed a pneumothorax. It may cause portion of the lung to collapse and occasionally problems breathing. If the air leak is tiny, it frequently heals better without any therapy. Large air leaks are addressed by putting a chest tube (a short tube into the chest area) which sucks out the air over a day or two, following which it normally heals on its own.
Bronchoscopy
Bronchoscopy may assist the doctor detect certain tumors or obstructions in the bigger airways of the lungs, which can frequently be biopsied during the operation.
Tests to identify lung cancer spread in the chest
Whether lung cancer has been diagnosed, it’s typically vital to know if it has progressed to the lymph nodes in the space between the lungs (mediastinum) or other surrounding locations. This might alter a person’s treatment choices. Several sorts of testing may be done to search for this cancer spread.
Endobronchial ultrasound
An endobronchial ultrasound may be used to see the lymph nodes and other structures in the space between the lungs if biopsies need to be obtained in those places.
Endoscopic esophageal ultrasound
An endoscopic esophageal ultrasonography penetrates down into the esophagus where it may reveal the adjacent lymph nodes which may contain lung cancer cells. Biopsies of the aberrant lymph nodes might be obtained at the same time as the surgery.
Mediastinoscopy and mediastinotomy
These techniques may be done to examine more directly at and acquire samples from the structures in the mediastinum (the space between the lungs) (the area between the lungs). The fundamental difference between the two is in the placement and size of the incision.
A mediastinoscopy is a technique that employs a lighted tube placed beneath the sternum (breast bone) and in front of the windpipe to look at and obtain tissue samples from the lymph nodes along the windpipe and the main bronchial tube locations. If certain lymph nodes can’t be reached by mediastinoscopy, a mediastinotomy may be done so the surgeon may directly extract the biopsy sample. For this treatment, a somewhat bigger incision (typically around 2 inches long) between the left second and third ribs adjacent to the breast bone is required.
Thoracoscopy
Thoracoscopy may be done to find out whether cancer has spread to the gaps between the lungs and the chest wall, or to the linings of these spaces. It may also be used to collect malignancies on the outer regions of the lungs as well as surrounding lymph nodes and fluid, and to check if a tumor is expanding into neighboring tissues or organs. This treatment is not commonly done simply to identify lung cancer, unless other procedures such as needle biopsies are unable to collect enough samples for the diagnosis. Thoracoscopy may also be performed as part of the therapy to remove part of a lung in certain early-stage lung malignancies. This form of procedure, known as video-assisted thoracic surgery (VATS), is discussed in Surgery for Non-Small Cell Lung Cancer.
Lung function tests
Lung (or pulmonary) function tests (PFTs) are commonly done when lung cancer is detected to determine how well your lungs are operating. This is particularly significant if surgery could be a possibility in treating the malignancy. Surgery to remove lung cancer may involve removing part or all of a lung, so it’s crucial to know how well your lungs are operating beforehand. Some persons with poor lung function (such those with lung damage from smoking) don’t have enough undamaged lung to resist removing even part of a lung. These tests may give the surgeon an indication of whether surgery is a suitable choice, and if so, how much lung can safely be removed.
There are many varieties of PFTs, but they all simply have you breathe in and out through a tube that is attached to a machine that analyzes airflow.
Sometimes PFTs are paired with a test called an arterial blood gas. In this test, blood is extracted from an artery (instead of from a vein, like most other blood tests) so the quantity of oxygen and carbon dioxide may be evaluated.
Lab examinations of biopsies and other samples
Samples that have been taken during biopsies or other testing are submitted to a pathology lab. A pathologist, a doctor who conducts lab tests to identify disorders such as cancer, will look at the samples and may undertake additional specific tests to assist better categorize the malignancy. (Cancers from other organs also may travel to the lungs. It’s really crucial to figure out where the cancer originated, since therapy is varied based on the kind of cancer.)
The findings of these tests are detailed in a pathology report, which is normally ready within a week. If you have any concerns regarding your pathology findings or other diagnostic testing, go to your doctor. If required, you may receive a second opinion on your pathology report by having your tissue samples forwarded to a pathologist at another lab.
Molecular assays for gene alterations
In certain circumstances, particularly for non-small cell lung cancer (NSCLC), physicians may screen for specific gene alterations in the cancer cells that might imply certain targeted medications can help treat the malignancy. For example:
- About 20 -25 percent of NSCLCs have mutations in the KRAS gene that lead them to create an aberrant KRAS protein which promotes the cancer cells grow and spread. NSCLCs with this mutation are typically adenocarcinomas, resistant to other medicines such as EGFR inhibitors, and are more commonly identified in patients with a smoking history.
- EGFR is a protein that exists in large concentrations on the surface of 10 percent to 20 percent of NSCLC cells and helps them proliferate. Some medications that target EGFR may be used to treat NSCLC with alterations in the EGFR gene, which are more frequent in particular demographics, such as those who don't smoke, women, and Asians. But these treatments don’t appear to be as useful in people whose cancer cells contain alterations in the KRAS gene.
- About 5 percent of NSCLCs contain an alteration in the ALK gene. This shift is most typically found in those who don't smoke (or who smoke lightly) who have the adenocarcinoma subtype of NSCLC. Doctors may screen tumours for alterations in the ALK gene to determine whether medications that target this mutation may benefit patients.
- About 1 percent to 2 percent of NSCLCs contain a rearrangement in the ROS1 gene, which could help the tumor react to specific targeted medicines.
- A tiny fraction of NSCLCs have mutations in the RET gene. Certain medications that target cells with RET gene alterations could be alternatives for treating these cancers.
- About 5 percent of NSCLCs contain mutations in the BRAF gene. Certain medications that target cells with BRAF gene alterations could be a possibility for treating these cancers.
- A tiny minority of NSCLCs contain particular mutations in the MET gene that make them more likely to react to certain targeted medicines.
These molecular tests may be done on tissue collected after a biopsy or surgery for lung cancer. If the biopsy sample is too tiny and all the molecular tests cannot be done, the testing may alternatively be done on blood that is collected from a vein much like a standard blood draw. This blood includes the DNA from dead tumor cells seen in the circulation of persons with advanced lung cancer. Obtaining the tumor DNA by a blood draw is frequently dubbed a "liquid biopsy" and may offer benefits over a traditional needle biopsy, which can involve dangers such a pneumothorax (lung collapse) and shortness of breath.
Tests for particular proteins on tumor cells
Lab tests could also be done to search for particular proteins on the cancer cells. For example, NSCLC cells could be checked for the PD-L1 protein, which might suggest whether the tumour is more likely to react to treatment with particular immunotherapy medications.
Blood tests
Blood tests are not used to identify lung cancer, but they may assist to obtain a sense of a person’s general health. For example, they may be used to assist evaluate whether a person is healthy enough to undergo surgery.
A complete blood count (CBC) checks at whether your blood contains normal levels of various kinds of blood cells. For example, it may reveal whether you are anemic (have a low number of red blood cells), if you might have difficulties with bleeding (due to a low number of blood platelets), or if you are at elevated risk for infections (because of a low number of white blood cells) (because of a low number of white blood cells). This test may be done often throughout therapy, since many cancer medications might alter blood-forming cells of the bone marrow.
Blood chemistry tests may help discover problems in certain of your organs, such as the liver or kidneys. For example, if cancer has spread to the bones, it could produce higher than usual levels of calcium and alkaline phosphatase.